McMillan JA, Land ML, Rodday AM, Wills K, Green CM, Leslie LK. Report of a joint association of pediatric program directors–American Board of Pediatrics Workshop: preparing future pediatricians for the mental health crisis. J Pediatr. 2018;201:285–91.
Google Scholar
Hoagwood KE, Kelleher KJ. A Marshall plan for children’s mental health after COVID-19. Psychiatr Serv. 2020;71:1216–7.
Google Scholar
Bitsko RH, Claussen AH, Lichstein J, Black LI, Jones SE, Danileson ML, et al. Mental health surveillance among children—United States, 2013–2019. MMWR Suppl. 2022;71:1–42.
U.S. DHHS. Advisory on social media and youth mental health: the U.S. Surgeon General’s Advisory. 2023. https://www.hhs.gov/sites/default/files/sg-youth-mental-health-social-media-advisory.pdf. Accessed August 10. U.S. DHHS; 2023.
CDC. Youth risk behavior surveillance data summary & trends report: 2011–2021. CDC; 2023.
Lindsey MA, Sheftall AH, Xiao Y, Joe S. Trends of suicidal behaviors among high school students in the United States: 1991–2017. Pediatrics. 2019;144:e20191187.
Google Scholar
Alegria M, Shrout PE, Canino G, Alvarez K, Wang Y, Bird H, et al. The effect of minority status and social context on the development of depression and anxiety: a longitudinal study of Puerto Rican descent youth. World Psychiatry. 2019;18:298–307.
Google Scholar
Lee M-J, Liechty JM. Longitudinal associations between immigrant ethnic density, neighborhood processes, and Latino immigrant youth depression. J Immigr Minor Health. 2015;17:983–91.
Google Scholar
Avenevoli S, Swendsen J, He J-P, Burstein M, Merikangas KR. Major depression in the national comorbidity survey-adolescent supplement: prevalence, correlates, and treatment. J Am Acad Child Adolesc Psychiatry. 2015;54:37–44.e2.
Google Scholar
Merikangas KR, He J-P, Burstein M, Swanson SA, Avenevoli S, Cui L, et al. Lifetime prevalence of mental disorders in U.S. adolescents: results from the National Comorbidity Survey Replication-Adolescent Supplement (NCS-A). J Am Acad Child Adolesc Psychiatry. 2010;49:980–9.
Google Scholar
McGrath JJ, Al-Hamzawi A, Alonso J, Altwaijri Y, Andrade LH, Bromet EJ, et al. Age of onset and cumulative risk of mental disorders: a cross-national analysis of population surveys from 29 countries. Lancet Psychiatry. 2023;10:668–81.
Google Scholar
Casey BJ, Jones RM, Levita L, Libby V, Pattwell SS, Ruberry EJ, et al. The storm and stress of adolescence: insights from human imaging and mouse genetics. Dev Psychobiol. 2010;52:225–35.
Google Scholar
Somerville LH. Special issue on the teenage brain: sensitivity to social evaluation. Curr Dir Psychol Sci. 2013;22:121–7.
Google Scholar
Sawyer SM, Azzopardi PS, Wickremarathne D, Patton GC. The age of adolescence. Lancet Child Adolesc Health. 2018;2:223–8.
Google Scholar
Blakemore S-J. Adolescence and mental health. Lancet. 2019;393:2030–1.
Google Scholar
Choukas-Bradley S, Kilic Z, Stout CD, Roberts SR. Perfect storms and double-edged swords: recent advances in research on adolescent social media use and mental health. Adv Psychiatry Behav Health. 2023;3:149–57.
Google Scholar
Vogels EA, Gelles-Watnick R, Massarat N. Teens, social media and technology 2022. Pew Research Center: Internet. Science & Tech;2022. https://www.pewresearch.org/internet/2022/08/10/teens-social-media-and-technology-2022/.
Anderson M, Jiang J. Teens, social media & technology 2018. Pew Res Center. 2018;31:1673–89.
Lenhart A. Teens, technology and friendships. Washington, DC: Pew Research Center; 2015.
Haidt J, Twenge JM. This is our chance to pull teenagers out of the smartphone trap. NY Times; 2021.
Leonhardt D. On the phone, alone. NY Times; 2022.
Bagot KS, Tomko RL, Marshall AT, Hermann J, Cummins K, Ksinan A, et al. Youth screen use in the ABCD® study. Dev Cogn Neurosci. 2022;57:101150.
Google Scholar
van Dijck J. The culture of connectivity: a critical history of social media. New York, NY: Oxford University Press; 2013.
Rideout V. The common sense census: media use by tweens and teens. Los Angeles: Common Sense Media; 2015.
Mojtabai R, Olfson M, Han B. National trends in the prevalence and treatment of depression in adolescents and young adults. Pediatrics. 2016;138:e20161878.
Google Scholar
Miron O, Yu K-H, Wilf-Miron R, Kohane IS. Suicide rates among adolescents and young adults in the United States, 2000-2017. JAMA. 2019;321:2362–4.
Google Scholar
Odgers CL, Jensen MR. Annual research review: adolescent mental health in the digital age: facts, fears, and future directions. J Child Psychol Psychiatry. 2020;61:336–48.
Google Scholar
Baker DA, Algorta GP. The relationship between online social networking and depression: a systematic review of quantitative studies. Cyberpsychol Behav Soc Netw. 2016;19:638–48.
Google Scholar
Ivie EJ, Pettitt A, Moses LJ, Allen NB. A meta-analysis of the association between adolescent social media use and depressive symptoms. J Affect Disord. 2020;275:165–74.
Google Scholar
Eirich R, McArthur BA, Anhorn C, McGuinness C, Christakis DA, Madigan S. Association of screen time with internalizing and externalizing behavior problems in children 12 years or younger: a systematic review and meta-analysis. JAMA Psychiatry. 2022;79:393–405.
Google Scholar
Nagata JM, Cortez CA, Cattle CJ, Ganson KT, Iyer P, Bibbins-Domingo K, et al. Screen time use among US adolescents during the COVID-19 pandemic. JAMA Pediatr. 2022;176:94.
Google Scholar
Paulich KN, Ross JM, Lessem JM, Hewitt JK. Screen time and early adolescent mental health, academic, and social outcomes in 9- and 10- year old children: Utilizing the Adolescent Brain Cognitive Development SM (ABCD) Study. PLoS ONE. 2021;16:e0256591.
Google Scholar
Paulus MP, Squeglia LM, Bagot K, Jacobus J, Kuplicki R, Breslin FJ, et al. Screen media activity and brain structure in youth: evidence for diverse structural correlation networks from the ABCD study. Neuroimage. 2019;185:140–53.
Google Scholar
Yoon S, Kleinman M, Mertz J, Brannick M. Is social network site usage related to depression? A meta-analysis of Facebook–depression relations. J Affect Disord. 2019;248:65–72.
Google Scholar
Riehm KE, Feder KA, Tormohlen KN, Crum RM, Young AS, Green KM, et al. Associations between time spent using social media and internalizing and externalizing problems among US youth. JAMA Psychiatry. 2019;76:1266–73.
Google Scholar
Twenge JM, Joiner TE, Rogers ML, Martin GN. Increases in depressive symptoms, suicide-related outcomes, and suicide rates among US adolescents after 2010 and links to increased new media screen time. Clin Psychol Sci. 2018;6:3–17.
Google Scholar
Steers M-LN, Wickham RE, Acitelli LK. Seeing everyone else’s highlight reels: how Facebook usage is linked to depressive symptoms. J Soc Clin Psychol. 2014;33:701–31.
Google Scholar
Heffer T, Good M, Daly O, MacDonell E, Willoughby T. The longitudinal association between social-media use and depressive symptoms among adolescents and young adults: an empirical reply to Twenge et al. (2018). Clin Psychol Sci. 2019;7:462–70.
Google Scholar
Orben A, Przybylski AK, Blakemore S-J, Kievit RA. Windows of developmental sensitivity to social media. Nat Commun. 2022;13:1649.
Google Scholar
Steinsbekk S, Nesi J, Wichstrøm L. Social media behaviors and symptoms of anxiety and depression. A four-wave cohort study from age 10–16 years. Comput Human Behav. 2023;147:107859.
Google Scholar
Coyne SM, Rogers AA, Zurcher JD, Stockdale L, Booth M. Does time spent using social media impact mental health?: An eight year longitudinal study. Comput Human Behav. 2020;104:106160.
Google Scholar
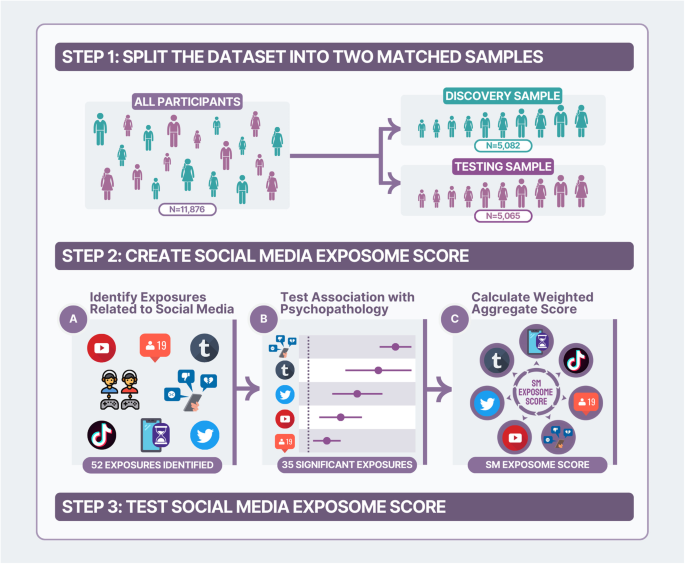
Moore TM, Visoki E, Argabright ST, Didomenico GE, Sotelo I, Wortzel JD, et al. Modeling environment through a general exposome factor in two independent adolescent cohorts. Exposome. 2022;2:osac010.
Google Scholar
Juarez PD, Matthews-Juarez P. Applying an Exposome-Wide (ExWAS) approach to cancer research. Front Oncol. 2018;8:313.
Google Scholar
Hosnijeh FS, Nieters A, Vermeulen R. Association between anthropometry and lifestyle factors and risk of B‐cell lymphoma: an exposome‐wide analysis. Int J Cancer. 2021;148:2115–28
Google Scholar
Vrijheid M, Fossati S, Maitre L, Márquez S, Roumeliotaki T, Agier L, et al. Early-life environmental exposures and childhood obesity: an exposome-wide approach. Environ Health Perspect. 2020;128:67009.
Google Scholar
Lin BD, Pries L-K, Sarac HS, van Os J, Rutten BPF, Luykx J, et al. Nongenetic factors associated with psychotic experiences among UK Biobank Participants: exposome-wide analysis and Mendelian randomization analysis. JAMA Psychiatry. 2022;79:857–68.
Google Scholar
Wild CP. The exposome: from concept to utility. Int J Epidemiol. 2012;41:24–32.
Google Scholar
Vrijheid M, Slama R, Robinson O, Chatzi L, Coen M, van den Hazel P, et al. The human early-life exposome (HELIX): project rationale and design. Environ Health Perspect. 2014;122:535–44.
Google Scholar
Poveda A, Pomares-Millan H, Chen Y, Kurbasic A, Patel CJ, Renström F, et al. Exposome-wide ranking of modifiable risk factors for cardiometabolic disease traits. Sci Rep. 2022;12:4088.
Google Scholar
Breslau J, Gilman SE, Stein BD, Ruder T, Gmelin T, Miller E. Sex differences in recent first-onset depression in an epidemiological sample of adolescents. Transl Psychiatry. 2017;7:e1139.
Google Scholar
Marshal MP, Dietz LJ, Friedman MS, Stall R, Smith HA, McGinley J, et al. Suicidality and depression disparities between sexual minority and heterosexual youth: a meta-analytic review. J Adolesc Health. 2011;49:115–23.
Google Scholar
Fox KR, Choukas-Bradley S, Salk RH, Marshal MP, Thoma BC. Mental health among sexual and gender minority adolescents: examining interactions with race and ethnicity. J Consult Clin Psychol. 2020;88:402–15.
Google Scholar
Kessler RC, McGonagle KA, Swartz M, Blazer DG, Nelson CB. Sex and depression in the National Comorbidity Survey. I: lifetime prevalence, chronicity and recurrence. J Affect Disord. 1993;29:85–96.
Google Scholar
Nagata JM, Singh G, Sajjad OM, Ganson KT, Testa A, Jackson DB, et al. Social epidemiology of early adolescent problematic screen use in the United States. Pediatr Res. 2022;92:1443–9.
Google Scholar
Gonzalez R, Thompson EL, Sanchez M, Morris A, Gonzalez MR, Feldstein Ewing SW, et al. An update on the assessment of culture and environment in the ABCD Study®: Emerging literature and protocol updates over three measurement waves. Dev Cogn Neurosci. 2021;52:101021.
Google Scholar
Zucker RA, Gonzalez R, Feldstein Ewing SW, Paulus MP, Arroyo J, Fuligni A, et al. Assessment of culture and environment in the Adolescent Brain and Cognitive Development Study: rationale, description of measures, and early data. Dev Cogn Neurosci. 2018;32:107–20.
Google Scholar
Barch DM, Albaugh MD, Avenevoli S, Chang L, Clark DB, Glantz MD, et al. Demographic, physical and mental health assessments in the adolescent brain and cognitive development study: rationale and description. Dev Cogn Neurosci. 2018;32:55–66.
Google Scholar
Volkow ND, Koob GF, Croyle RT, Bianchi DW, Gordon JA, Koroshetz WJ, et al. The conception of the ABCD study: from substance use to a broad NIH collaboration. Dev Cogn Neurosci. 2018;32:4–7.
Google Scholar
Garavan H, Bartsch H, Conway K, Decastro A, Goldstein RZ, Heeringa S, et al. Recruiting the ABCD sample: design considerations and procedures. Dev Cogn Neurosci. 2018;32:16–22.
Google Scholar
Achenbach TM, McConaughy SH, Ivanova MY, Rescorla LA. Manual for the ASEBA brief problem monitor (BPM). 33. Burlington, VT:ASEBA;2011.
Achenbach TM, Edelbrock C. Child behavior checklist. Burlington (Vt). 1991;7:371–92.
Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, et al. Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry. 1997;36:980–8.
Google Scholar
Townsend L, Kobak K, Kearney C, Milham M, Andreotti C, Escalera J, et al. Development of three web-based computerized versions of the kiddie schedule for affective disorders and schizophrenia child psychiatric diagnostic interview: preliminary validity data. J Am Acad Child Adolesc Psychiatry. 2020;59:309–25.
Google Scholar
Hoffman EA, Clark DB, Orendain N, Hudziak J, Squeglia LM, Dowling GJ. Stress exposures, neurodevelopment and health measures in the ABCD study. Neurobiol Stress. 2019;10:100157.
Google Scholar
R Core Team, R. R: A language and environment for statistical computing. R Core Team, R;2013.
Pries L-K, Moore TM, Visoki E, Sotelo I, Barzilay R, Guloksuz S. Estimating the association between exposome and psychosis as well as general psychopathology: results from the ABCD study. Biol Psychiatry Glob Open Sci. 2022;2:283–91.
Google Scholar
Barzilay R, Moore TM, Calkins ME, Maliackel L, Jones JD, Boyd RC, et al. Deconstructing the role of the exposome in youth suicidal ideation: Trauma, neighborhood environment, developmental and gender effects. Neurobiol Stress. 2021;14:100314.
Google Scholar
Patel CJ. Introduction to environment and exposome-wide association studies: a data-driven method to identify multiple environmental factors associated with phenotypes in human populations. n: Rider CV, Simmons JE, editors. Chemical mixtures and combined chemical and nonchemical stressors. Basel: Springer International Publishing; 2018. p. 129–49.
Feczko E, Conan G, Marek S, Tervo-Clemmens B, Cordova M, Doyle O, et al. Adolescent brain cognitive development (ABCD) community MRI collection and utilities. bioRxiv:2021.07.09.451638v1 [Preprint]. 2021 [cited 2021 Jul 11]: [33 p.]. Available from: https://www.biorxiv.org/content/10.1101/2021.07.09.451638v1.
Stekhoven DJ, Bühlmann P. MissForest—non-parametric missing value imputation for mixed-type data. Bioinformatics. 2012;28:112–8.
Google Scholar
Kuhn M. Building predictive models in R using the caret package. J Stat Softw. 2008;28:1–26.
Google Scholar
Bates D, Mächler M, Bolker B, Walker S. Fitting linear mixed-effects models using lme4. arXiv [StatCO]. 2014.
Nakagawa S, Johnson PCD, Schielzeth H. The coefficient of determination R2 and intra-class correlation coefficient from generalized linear mixed-effects models revisited and expanded. J R Soc Interface. 2017;14:20170213.
Google Scholar
Gordon JH, Tran KT, Visoki E, Argabright S, DiDomenico GE, Saiegh E, et al. The role of individual discrimination and structural stigma in the mental health of sexual minority youth. J Am Acad Child Adolesc Psychiatry. 2023;5. https://doi.org/10.1016/j.jaac.2023.05.033.
VanderWeele TJ, Ding P. Sensitivity analysis in observational research: Introducing the E-value. Ann Intern Med. 2017;167:268–74.
Google Scholar
Brunstein Klomek A, Marrocco F, Kleinman M, Schonfeld IS, Gould MS. Bullying, depression, and suicidality in adolescents. J Am Acad Child Adolesc Psychiatry. 2007;46:40–9.
Google Scholar
Holt MK, Vivolo-Kantor AM, Polanin JR, Holland KM, DeGue S, Matjasko JL, et al. Bullying and suicidal ideation and behaviors: a meta-analysis. Pediatrics. 2015;135:e496–509.
Google Scholar
Klomek AB, Sourander A, Gould M. The association of suicide and bullying in childhood to young adulthood: a review of cross-sectional and longitudinal research findings. Can J Psychiatry. 2010;55:282–8.
Google Scholar
Ruch DA, Heck KM, Sheftall AH, Fontanella CA, Stevens J, Zhu M, et al. Characteristics and precipitating circumstances of suicide among children aged 5 to 11 years in the United States, 2013-2017. JAMA Netw Open. 2021;4:e2115683.
Google Scholar
Nagata JM, Singh G, Yang JH, Smith N, Kiss O, Ganson KT, et al. Bedtime screen use behaviors and sleep outcomes: findings from the Adolescent Brain Cognitive Development (ABCD) Study. Sleep Health; 2023. https://doi.org/10.1016/j.sleh.2023.02.005.
Bernert RA, Kim JS, Iwata NG, Perlis ML. Sleep disturbances as an evidence-based suicide risk factor. Curr Psychiatry Rep. 2015;17:554.
Google Scholar
Pigeon WR, Pinquart M, Conner K. Meta-analysis of sleep disturbance and suicidal thoughts and behaviors. J Clin Psychiatry. 2012;73:e1160–7.
Google Scholar
Liu RT, Steele SJ, Hamilton JL, Do QBP, Furbish K, Burke TA, et al. Sleep and suicide: a systematic review and meta-analysis of longitudinal studies. Clin Psychol Rev. 2020;81:101895.
Google Scholar
Verduyn P, Gugushvili N, Kross E. The impact of social network sites on mental health: distinguishing active from passive use. World Psychiatry. 2021;20:133–4.
Google Scholar
Escobar-Viera CG, Shensa A, Bowman ND, Sidani JE, Knight J, James AE, et al. Passive and active social media use and depressive symptoms among United States adults. Cyberpsychol Behav Soc Netw. 2018;21:437–43.
Google Scholar
Frison E, Eggermont S. Exploring the relationships between different types of Facebook use, perceived online social support, and adolescents’ depressed mood. Soc Sci Comput Rev. 2016;34:153–71.
Google Scholar
Conley CS, Rudolph KD. The emerging sex difference in adolescent depression: interacting contributions of puberty and peer stress. Dev Psychopathol. 2009;21:593–620.
Google Scholar
Sheftall AH, Vakil F, Ruch DA, Boyd RC, Lindsey MA, Bridge JA. Black youth suicide: investigation of current trends and precipitating circumstances. J Am Acad Child Adolesc Psychiatry. 2022;61:662–75.
Google Scholar
Gordon J. Addressing the crisis of Black youth suicide. Health. 2020;2019:2018.
Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull. 2003;129:674–97.
Google Scholar
Frost DM, Meyer IH. Minority stress theory: application, critique, and continued relevance. Curr Opin Psychol. 2023;51:101579.
Google Scholar
Barzilay R, Pries L-K, Moore TM, Gur RE, van Os J, Rutten BPF, et al. Exposome and trans-syndromal developmental trajectories toward psychosis. Biol Psychiatry Glob Open Sci. 2022;2:197–205.
Google Scholar
Chancellor S, De Choudhury M. Methods in predictive techniques for mental health status on social media: a critical review. NPJ Digit Med. 2020;3:43.
Google Scholar
Nguyen VC, Lu N, Kane JM, Birnbaum ML, De Choudhury M. Cross-platform detection of psychiatric hospitalization via social media data: comparison study. JMIR Ment Health. 2022;9:e39747.
Google Scholar
Allen NB, Nelson BW, Brent D, Auerbach RP. Short-term prediction of suicidal thoughts and behaviors in adolescents: can recent developments in technology and computational science provide a breakthrough? J Affect Disord. 2019;250:163–9.
Google Scholar
Yau JC, Reich SM. Are the qualities of adolescents’ offline friendships present in digital interactions? Adolesc Res Rev. 2018;3:339–55.
Ellis WE, Dumas TM, Forbes LM. Physically isolated but socially connected: psychological adjustment and stress among adolescents during the initial COVID-19 crisis. Can J Behav Sci. 2020;52:177.
Google Scholar
Hamilton JL, Dreier MJ, Boyd SI. Social media as a bridge and a window: the changing relationship of adolescents with social media and digital platforms. Curr Opin Psychol. 2023;52:101633.
Google Scholar
Klassen S. Black Twitter is gold: why this online community is worthy of study and how to do so respectfully. Interactions. 2022;29:96–98.
Google Scholar
Clark MD. To tweet our own cause: a mixed-methods study of the online phenomenon “Black Twitter.” Chapel Hill, NC: The University of North Carolina at Chapel Hill Graduate School; 2014.
Fox J, Ralston R. Queer identity online: Informal learning and teaching experiences of LGBTQ individuals on social media. Comput Human Behav. 2016;65:635–42.
Google Scholar
Craig SL, Eaton AD, McInroy LB, Leung VWY, Krishnan S. Can social media participation enhance LGBTQ+ youth well-being? Development of the Social Media Benefits Scale. Social Media + Society. 2021;7:2056305121988931.
Google Scholar
Craig SL, McInroy L, McCready LT, Alaggia R. Media: a catalyst for resilience in Lesbian, Gay, Bisexual, Transgender, and Queer Youth. J LGBT Youth. 2015;12:254–75.
Google Scholar
Lees B, Squeglia LM, Breslin FJ, Thompson WK, Tapert SF, Paulus MP. Screen media activity does not displace other recreational activities among 9-10 year-old youth: a cross-sectional ABCD study®. BMC Public Health. 2020;20:1783.
Google Scholar
APA. APA chief scientist outlines potential harms, benefits of social media for kids. American Psychological Association; 2023. https://www.apa.org/news/press/releases/2023/02/harms-benefits-social-media-kids?utm_source=twitter&utm_medium=social&utm_campaign=apa-press-release-research&utm_content=feb14-prinstein-testimony.
Stockdale LA, Coyne SM. Bored and online: Reasons for using social media, problematic social networking site use, and behavioral outcomes across the transition from adolescence to emerging adulthood. J Adolesc. 2020;79:173–83.
Google Scholar
Bagot KS, Matthews SA, Mason M, Squeglia LM, Fowler J, Gray K, et al. Current, future and potential use of mobile and wearable technologies and social media data in the ABCD study to increase understanding of contributors to child health. Dev Cogn Neurosci. 2018;32:121–9.
Google Scholar
Wade NE, Ortigara JM, Sullivan RM, Tomko RL, Breslin FJ, Baker FC, et al. Passive sensing of preteens’ smartphone use: an Adolescent Brain Cognitive Development (ABCD) Cohort Substudy. JMIR Ment Health. 2021;8:e29426.
Google Scholar